Urogynaecology
Urogynaecology
Provision of optimum care for women suffering from pelvic floor dysfunction which include urinary and anal incontinence, pelvic organ prolapse, obstetric anal sphincter injury (OASIS), voiding, defecatory and sexual dysfunction.
Provision of evidence based medical practice in Urogynaecology to improve the quality of life in women with pelvic floor dysfunction, via promoting research.
Provision of optimum pelvic floor care and training ground for Urogynaecology related expertise.
• Generally, to provide optimum care for patients with pelvic floor dysfunctions.
• Specifically :
To provide patient education regarding care of the pelvic floor.
To provide management plan for women with pelvic floor dysfunction.
To provide management plan and care for women post-repair of OASIS.
To provide conservative treatment for pelvic dysfunction, through combined care with pelvic floor physiotherapist and other related disciplines such as colorectal team.
To provide preoperative counselling for women with pelvic floor dysfunction (who failed / not fit / declined conservative treatment), planned for surgical intervention.
To provide complete and appropriate preoperative assessment which is not limited to urodynamics study and pelvic floor imaging.
To provide surgical intervention necessary for the treatment of pelvic floor dysfunctions
To provide appropriate post-operative care and to manage post-operative complications in the short or long term.
To provide subspecialty training for O&G specialist (local and international candidates)
To act as a referral centre for urogynaecology and post-repair of OASIS in the region.
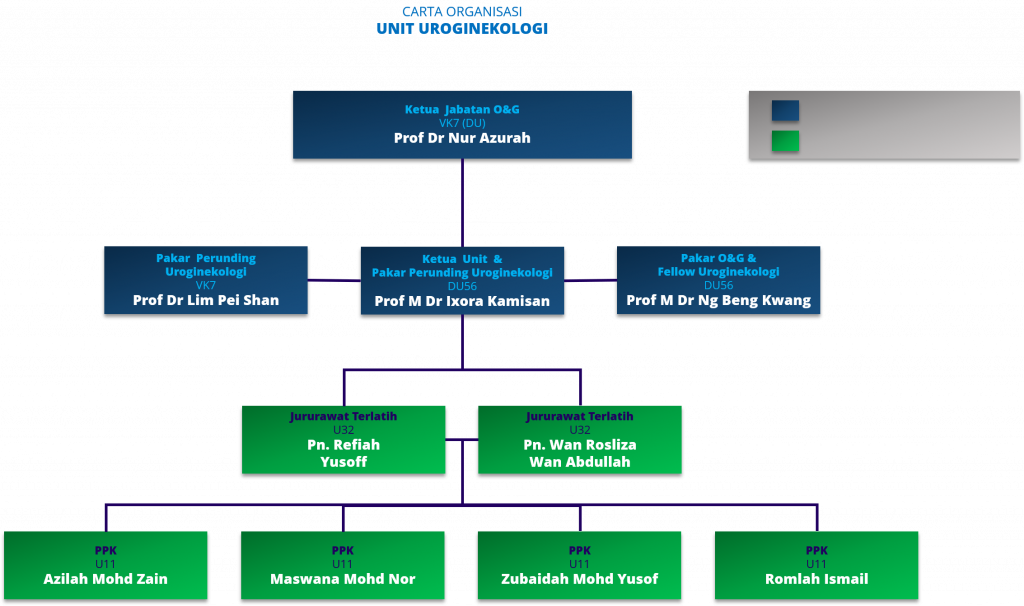
Organization Chart
Services
1. Facilitate the provision of Urogynaecology services to patients in the Facility in a safe, efficient, effective and caring manner and with due regard for the needs, dignity and privacy of patients and confidentiality of their personal information.
2. Assure continuity of care.
3. Address the professional needs of the medical practitioners.
4. Ensure that the medical practitioners are involved in the formulation of policies and procedures concerning patient care appropriate to the scope of services of the Facility.
5. Manage women with pelvic floor dysfunction which include pelvic organ prolapse, urinary and anal incontinence, voiding, defaecatory and sexual dysfunction.
6. Assure continuity of follow-up for women who had pelvic reconstructive or anti-incontinence surgery.
1. Women who had sustained major maternal birth trauma will be managed by in this clinic.
a. Obsteric anal sphincter injury (OASIS)
b. Intrapartum extended vaginal tear.
c. Obstetric fistula or postoperative complication fistula.
2. A venue for debriefing women who sustained major intrapartum maternal birth trauma.
3. Pelvic floor and anal sphincter imaging.
4. All referrals to perineal clinic should be discussed with urogynaecology consultants.
5. Women post-OASIS or major tear is seen at 8 weeks postpartum onwards, unless symptomatic.
1. All referrals must be directed to the urogynaecology consultants or fellow.
2. Urodynamic study may be performed in such situations:
a. If a diagnosis cannot be reached following a full continence assessment.
b. Failed initial treatment for continence.
c. To increase diagnostic accuracy above that which can be achieved by non-urodynamic means.
d. To make a clinical observation on which a management plan can be based.
e. To prioritise treatment in women with multiple pelvic floor dysfunctions.
f. To define the current situation, creating a baseline for future surveillance.
g. To predict problems that may follow treatment interventions, thus facilitate patient counselling prior to treatment.
h. To exclude abnormalities which may interfere with the management of that patient.
i. To assess the results of treatments designed to affect lower urinary tract function.
j. When surgical intervention / invasive procedure is being considered.
1. All referrals should be directed to the urogynaecology consultants or fellow.
2. This ultrasound examination is for women :
a. Planned for surgical intervention of pelvic organ prolapse.
b. Planned for anti-incontinence surgery.
c. Voiding dysfunction or obstructed defaecation.
d. Recurrent urinary tract infection.
e. Suspected urethral diverticulum.
f. Suspected vesico-vaginal or rectovaginal fistulae.
g. Women who had repair or OASIS / extended vaginal wall tear.
h. Assessment of recurrent prolapse.
i. Post-op assessment / surveillance.

